 A new artificial womb-like device may transform care for extremely premature infants: After birth, they would be immersed in lab-made amniotic fluid — and kept underwater for weeks.
A new artificial womb-like device may transform care for extremely premature infants: After birth, they would be immersed in lab-made amniotic fluid — and kept underwater for weeks.
When a premature baby is born three or even four months early, it’s immediately clear that they’re not ready to be here yet. Born at a critically low birth weight, the first challenge these very preterm babies face is surviving. Those that do survive face very serious challenges as they grow and develop. Many infants born preterm have severe, long-lasting medical complications or health problems. These premature infants present a real clinical challenge. New research hopes to help these babies who struggle to survive.
In the United States, the number of infants born significantly premature (sometimes called micro preemies) has increased over the past two to three decades. Infant mortality (death) of babies born around 23 to 24 weeks is around 50 percent. For those preterm infants that do survive, the majority will have some sort of illness, often due to lung immaturity. Despite great advances in care and technology, clinicians face great challenges in saving these babies and then helping them overcome health problems as they grow.
Many research studies have explored new ways to care for the preterm infant, with limited success. In the latest research from Children’s Hospital of Philadelphia, researchers changed their approach to think of a critically premature baby as a fetus, instead of as a newborn baby.
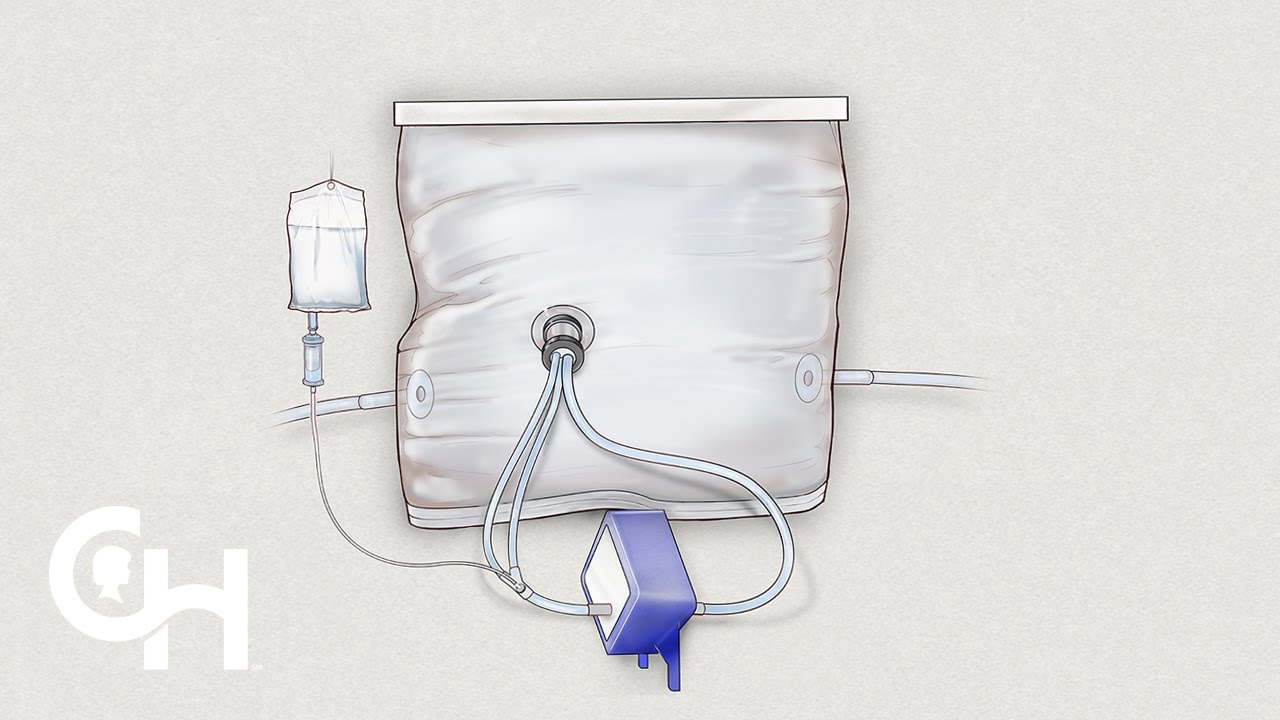
In this video, researchers and clinicians from Children’s Hospital of Philadelphia talk about an extra-uterine device that recreates the womb.
The device works by works by two major components. First, a circulatory system that allows the baby to get oxygen through the blood (rather than through the lungs), just like in the womb. This is a process called oxygenation. The other component is a fluid environment – the fetus is enclosed in heavy-duty bag filled with lab-made amniotic fluid.
Researchers Emily Partridge, MD, PhD, and Marcus Davey, PhD; neonatologist Kevin Dysart, MD; and pediatric and fetal surgeon and director of the Center for Fetal Research, Alan Flake, MD, talk about the evolution of this research and their hope to translate this system into a clinical therapy for human babies.
In the future, the team hopes to see the device become an innovative solution used in neonatal intensive care units to support extremely premature infants, such as a 23 or 24 week old baby who is faced with extreme challenges adapting to life outside the uterus.
http://www.chop.edu/news/unique-womb-...
Recreating the Womb: New Hope for Premature Babies health insurance | |
| 720 Likes | 720 Dislikes |
| 239,702 views views | 89.3K followers |
| Science & Technology | Upload TimePublished on 25 Apr 2017 |
No comments:
Post a Comment